If you do any research these days into your refractive surgery options, you will inevitably see the terms “LASEK”, “PRK” and occasionally “advanced surface ablation” (ASA) being batted around. What is PRK, what’s LASEK, what is the difference, and how does ASA relate to these?
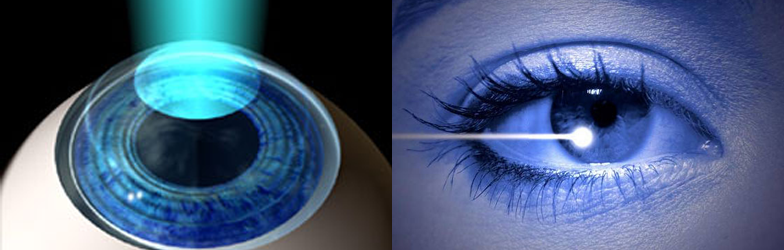
First, very simply, the above procedures reshape the cornea to reduce or eliminate your need for glasses and contacts just like LASIK and Intralase do, but they do so without creating a flap. With PRK and LASEK, the reshaping of your cornea takes place just under the thin loose surface layer of your cornea, called the epithelium. In both procedures, a contact lens is placed on the eye to protect the new cells as the heal.
LASEK OVERVIEW
A lot of the information available to you on the internet regarding LASEK is at the very least confusing, so I think it’s important that you get the facts, based on peer-reviewed studies and clinical experience that have guided thoughtful surgeons over the last decade on this subject.
Terminology
PRK stands for “photo-refractive keratectomy” while LASEK stands for “laser assisted epithelial keratectomy” ( the last word, “keratectomy”, which means removal of corneal tissue, being used in favor of the original descriptive term given to the LASEK acronym “keratomileusis”, meaning “to manipulate within.”
A Brief History
LASEK was first coined by surgeon, Dr Massimo Camellin of Italy, who first described the LASEK procedure in 1998, and he and early pioneers like Dr. Shah in the UK were hopeful over 15 years ago that it might produce improved healing and less risk of corneal haze (scarring.)
More recently, “LASEK with Epithelial flap removal”, which is, in fact, PRK by another name, is now widely recognized as providing not just better initial vision than traditional LASEK during the 3–4 day epithelial healing period, but often significantly less pain than was observed in LASEK patients who had their epithelial flaps replaced back over their corneas. One of the better studies demonstrating this was conducted by Liu et al and appears in Cellular Biochemistry and Biophysics, May 2010 issue and involved one-year follow-up of over 1000 eyes.
The Procedure behind LASEK and PRK
Let’s look at how LASEK and PRK differ in terms of how the treatments are performed:
PRK procedure
- The surface cells (epithelium) are removed either with a high-speed mechanical brush, with diluted alcohol, or with the excimer laser itself (trans- epithelial), and the laser then reshapes the stronger layer underneath (the stroma). More recently, some surgeons performing LASEK may use an epithelial micro-keratome to mechanically separate the surface layer from the stroma (deeper layer) and then remove or, less frequently, replace this thin surface layer following the laser reshaping.
Historic LASEK procedure
- The surface cells were loosened with a diluted alcohol solution and then moved to the side in one sheet, away from the pupil. After the same laser treatment which one would have in PRK, the epithelial sheet of now non-viable surface cells were replaced back over the pupil to cover as well as could be their original position on the cornea.
Comparing PRK and LASEK
There are two main differences when comparing PRK vs LASEK that are observable both in the procedures themselves and how they affect patients that undergo these treatments.
-
Epithelial Flap Replacement
What was observed when comparing the 2 methods was that replacing the epithelial flap back over the pupil frequently caused delayed and irregular healing of the surface layer and the vision patients had while this healing was taking place was frequently worse than that of their counterparts who had PRK or “LASEK with flap removal, which has become preferred over the old LASEK method, for the above reasons.
-
Post-Operative Pain
Post-operative pain during the first 3 days after traditional LASEK was often found to be worse than after PRK. The theory behind this is that the dead epithelial cells may trap cytokines and other biproducts of cell death which may create a greater inflammatory reaction on the cornea, contributing to increased pain perception as well as a delayed/irregular healing process. Others have postulated that some of the diluted alcohol might remain in some concentration within the retained flap, which could further irritate the eye if replaced on the corneal surface.
Keep in mind, however, that newer LASEK techniques which involve the use of an epithelial micro-keratome may allow for increased cell viability and thus not create the increased post op pain that was frequently seen in alcohol-assisted LASEK, especially if the flap had been replaced.
The Current Stance on LASEK?
So why was traditional LASEK embraced by a host of surgeons 10–15 years ago, and then quickly abandoned by most surgeons? The hope was that LASEK might reduce the risk of corneal haze beyond PRK, which before the more consistent use of mitomycin (an anti-scarring agent) and better post-operative topical steroid regimens, was a more significant and feared problem with surface ablations. However, the risk of haze was not found to be improved after many comparison studies between LASEK and PRK , and now the risk of haze after surface ablation is very low, especially if patients follow their post operative regimen.
Through years of refinement, experienced surgeons obtain wonderful outcomes using an Amoils brush PRK technique or a “LASEK with epithelial flap removal” technique. We at Diamond Vision generally prefer Amoils brush PRK, which when coupled with a customized wavefront-guided or topography-guided treatment produces phenomenal results, and is referred to as advanced service ablation.
As always, we look forward to helping guide you in your decision-making as you determine the best vision correction procedures for you! We are proud to recommend our specialists at the Atlanta Eye Surgery Center to help you with your needs.
Contact Us
If you have more questions about LASIK procedures, get in touch with us.
Related Blogs

Timing is Everything: When to Consider LASIK After Nursing for Optimal Results
Timing is everything when considering LASIK eye surgery after nursing, and understanding the optimal period for this procedure is vital for both mother and baby.

Cataract Surgery: Restoring Clarity and Confidence
Cataract surgery is a transformative procedure that offers a new lease on clear vision and renewed confidence. As cataracts cloud the eye’s lens, causing blurred
Intralase LASIK Explained: What to Expect Before, During, and After the Procedure
Intralase LASIK is a cutting-edge procedure that offers a safe, effective, and precise way to enhance vision compared to traditional LASIK methods. Understanding what to
